|
GBSInsider’s online data analytics platform and print-on-demand
reports, supplemented by information provided by your claims
administrator and GBS advisor, will take an inside look into
your company’s information to relieve you from burdensome guesswork
and empower you with the answers and confidence you need to
make the best decisions in allocating your healthcare dollars.
For more information on GBSInsider, please contact your GBS
advisor or visit www.gallagherbenefits.com.
|
Demographic Reports Details
|
|
Report Name
|
Definition
|
|
Age-Sex Analysis Report categories
|
Compares the group's age and sex cohorts with the benchmark
population and develops a composite Age.Sex factor for the group
to tailor benchmark data
|
|
Age-Sex Factor Trend Report
|
Tracks historical changes over time in the group's population
size and Age-Sex factor
|
|
Enrollment by Member Relationship
|
Compares the group's distribution of members by type (employee,
spouse, child) with the benchmark population to illustrate potential
adverse selection by spouses or possible existence of enrolled
ineligible children
|
|
Membership Count
|
Shows the group's historical monthly count of employees and
dependents
|
|
Member Turnover Report
|
Details the members joining and leaving and the average turnover
for a given timeframe
|
|
Financial Reports Details
|
Report Name
|
Definition
|
|
Incurred Claims Report
|
Shows the group's estimated monthly incurred claims dollars
and PMPM costs
|
|
Paid Claims Report
|
Shows the group's monthly paid claims dollars and PMPM costs
|
|
Trend Analysis Report
|
Shows the group's rolling 12-month and 3-month average PMPM
costs used to determine emerging PMPM cost trends
|
|
Network Savings Report
|
Shows the group's in- vs. out-of-network claim utilization and
network savings amounts to monitor savings and provide the basis
for assessing actual discounts compared to a vendor's performance
standard
|
|
Claims Summary Report
|
Shows the group's claim dollars and number of claimants by claims
dollar amount categories
|
Utilization Reports Details
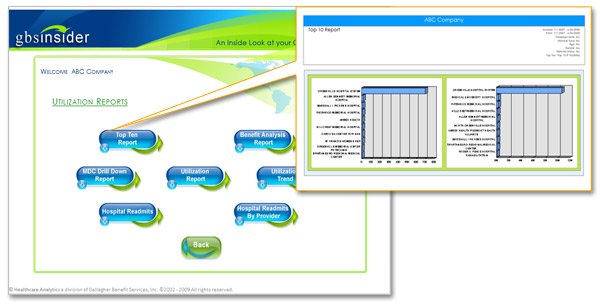
|
Report Name
|
Definition
|
|
Top Ten Report
|
Shows the group's top costs and services available in a large
number of medical service categories
|
|
Benefit Analysis Report
|
Shows the disposition of the group's covered claim amounts including
discounts, co-pays and deductibles, coinsurance, and coordination
of benefits adjustments
|
|
MDC Drill Down Report
|
Shows the group's hospital inpatient cost data grouped by Major
Diagnostic Category
|
|
Utilization Report
|
Shows the group's in- and out-of-network unit cost and utilization
data compared to custom benchmarks in as many as 40 user-defined
medical service categories
|
|
Utilization Trend
|
Provides the user with group's utilization data for exporting
to Excel for the calculation of the group's emerging medical
service utilization trends
|
|
Hospital Readmits Report
|
Analyzes the Hospital Re-Admits (30,60 and 90 Day) by Diagnosis
for the population.
|
|
Hospital Readmits By Provider Report
|
Analyzes the Hospital Re-Admits (30,60 and 90 Day) by Provider
for the population.
|
|
Advancing Imaging Utilization Report
|
...........
|
|
Advancing Imaging Analysis Report
|
...........
|
Benchmark Reports Details

|
Report Name
|
Definition
|
|
Benchmark Report
|
Shows a graphic comparison of the group's medical service unit
cost and utilization per 1,000 in any of up to 40 user defined
medical service categories compared to the benchmark population
|
|
|
|
|
|
|
|
|
|
Clinical Risk Groups (CRG) Reports Details
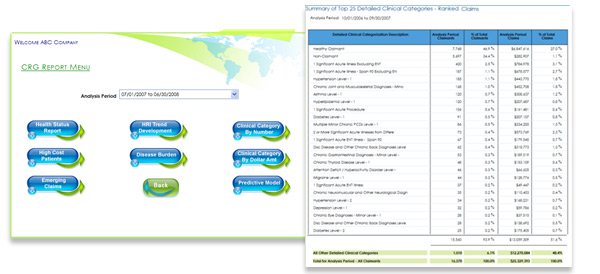
|
Report Name
|
Definition
|
|
Health Status Report
|
Shows the group's actual paid claims in 39 clinical risk groupings
as well as the health risk index (HRI) for each grouping compared
to the benchmark index
|
|
HRI Trend Development
|
Shows the group's retrospective (current period) and prospective
(following 12 months) health risk index in 39 clinical risk
groupings, as well as a composite HRI, used to predict the overall
change in the group's health status
|
|
HRIPopulation Report
|
Displays the group’s PMPM Cost, Retrospective and Prospective
Health Risk for given timeframe broken out by Acute and Chronic
Clinical Category Descriptions.
|
|
Potential High Cost Members
|
For members covered in the last month of the current analysis
period, shows the group's top 100 predicted claimants ranked
by claim amount for the 12 months following the current period
|
|
Disease Burden
|
Compares the group's actual distribution of non-healthy claimants
by major clinical category compared to the benchmark population
|
|
Clinical Category by Dollar Amount
|
Shows the group's top 25 clinical risk groups ranked by claim
dollar amount
|
|
Potential Emerging ClaimsReport
|
Displays the top 25 Potential Clinical Categories and Claims
Paid. The claims are ranked by the Future 12 Months claims.
|
|
Clinical Analysis Report
|
Compares Clinical conditions against benchmarks for the population.
|
|
Predictive Model
|
Evaluates the latest population's retrospective (current period)
and prospective (following 12 months) health risk index in 39
clinical risk groupings, as well as a composite HRI, used to
identify high-cost diagnoses that, in turn, provide a risk score
indicative of the likelihood to utilize more healthcare resources
and dollars than persons of the same age and gender.
|
|
Clinical Category by Number
|
Shows the group's top 25 clinical risk groups ranked by number
of claimants
|
Patient Level Reports Details
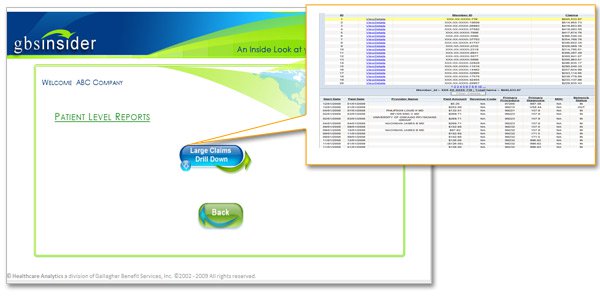
|
Report Name
|
Definition
|
|
Large Claim Drill Down
|
Shows a user-defined high dollar claimant listing for the group
with ability to drill down into claim details
|
|
Top 20 Large Claims Details Report
|
Displays the Top 20 high dollar claimants for the group and
allows you to drill-down and export the top 20 claims paid for
the group selected.
|
|
|
|
|
|
|
Experience Summary Reports Details

|
Report Name
|
Definition
|
|
Healthcare Benchmarking
|
Produces standard report without custom analysis ready for printing
containing preset report categories
|
|
Variance Analysis
|
Displays the variance between the benchmarks and actuals and
provides recommendations based upon the variance
|
|
|
|
|
|
|
Prescription Drug Reports Details
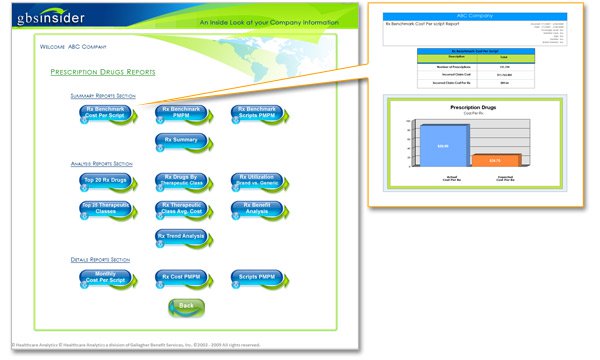
|
Report Name
|
Definition
|
|
Rx Benchmark Cost Per Script
|
Compares the group’s average Incurred Cost per Rx versus the
Benchmark.
|
|
Rx Benchmark PMPM
|
Shows the group's average Per Member per Month Incurred Cost
compared to the benchmark for the given population.
|
|
RX Benchmark Scripts PMPM
|
Compares the population’s average scripts per member versus
the benchmark.
|
|
Rx Summary
|
Compares the group's Rx cost and utilization by Brand/Generic,
and Retail/Mail-Order cohorts
|
|
Top 20 Rx Drugs Report
|
Compares the top 20 Rx Drugs prescribed with all other drugs
prescribed for the population
|
|
Rx Drugs By Therapeutic Class Report
|
Summarizes the top 25 Rx Drugs by Therapeutic Class, Brand/Generic,
Total Paid, Percentage of Total Rx Paid, Number of Scripts and
Total Prescriptions.
|
|
Rx Utilization Brand vs. Generic Report
|
Compares Total Prescriptions, Paid and Copay Amount by Drug
Type (Brand/Generic) for the selected population
|
|
Top 25 Therapeutic Classes Report
|
Summarizes up to the top 25 Therapeutic Classes and displays
the Total Paid and Total Prescriptions.
|
|
Rx Therapeutic Class Avg. Cost Report
|
Summarizes the Paid Amount, Rx Scripts and Average Costs for
the Top 25 Therapeutic Classes.
|
|
Rx Benefit Analysis
|
Shows the composition of the group's monthly Rx total and PMPM
claim costs including ingredient cost, dispensing fee, sales
tax, co-pay, and discount.Added a stacked bar graph displaying
the breakdown of Sales Tax, Ingredient Cost, Dispensing Fee
and Copay amount.
|
|
Rx Trend Analysis Report
|
Compares the PMPM, Rolling 3 and 12 month PMPM Claims and Trends
|
|
Specialty Rx Drug Report
|
Shows top 20 Details of 'Chemotherapy Drugs','Drugs Administered
Other than Oral Method' and 'Miscellaneous Drugs and Solution'(Specialty
Drugs Category).
|
|
Monthly Cost Per Script Report
|
Compares the monthly average Incurred Cost per Rx versus the
Benchmark
|
|
Rx Cost PMPM Report
|
Displays the monthly average Rx PMPM cost compared to the benchmark.
|
|
Script PMPM Report
|
Displays the average monthly Prescriptions per Member versus
the benchmark.
|
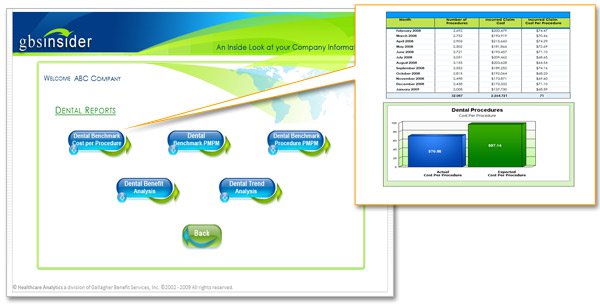
Dental Reports Details
|
Report Name
|
Definition
|
|
Dental Benchmark Cost per Procedure
|
Shows the group's average cost per dental procedure compared
to the benchmark population
|
|
Dental Benchmark PMPM
|
Shows the group's average dental PMPM cost compared to the benchmark
population
|
|
Dental Benchmark Procedure PMPM
|
Shows the group's average number of dental services per 1,000
members compared to the benchmark population
|
|
Dental Benefit Analysis
|
Shows the disposition of the group's covered dental claim amounts
including discounts, co-pays and deductibles, coinsurance, and
coordination of benefits adjustments
|
|
Dental Trend Analysis
|
Shows the group's rolling 12-month and 3-month average dental
PMPM costs used to determine emerging PMPM cost trends
|
|
Dental Membership Count
|
Shows the group's historical monthly count of employees and
dependents with dental coverage
|
Vision Reports Details

|
Report Name
|
Definition
|
|
Vision PMPM Report
|
Compares the population’s average vision costs per member versus
the benchmark.
|
|
Vision Cost Per Services
|
Compares the group’s average Incurred Cost per Service.
|
|
Vision Services PMPM
|
Compares the population’s average services costs per member
versus the benchmark.
|
|
Vision Benefit Analysis
|
Shows the disposition of the group's covered Vision claim amounts
including discounts, co-pays and deductibles, coinsurance, and
coordination of benefits adjustments
|
|
Vision Utilization
|
Displays the average number of services per 1000 and the average
costs per service.
|
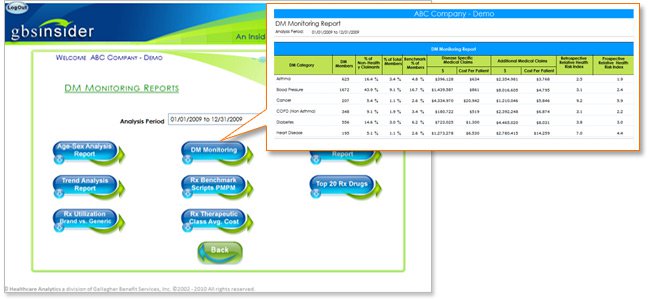
DM Monitoring Reports Details
The Disease Monitoring section contains a series of reports
designed to identify the demographics, health status, medical
resource utilization, and cost associated with members who have
been diagnosed with major health conditions that are chronic
in nature and many times related to lifestyles. The conditions
include Asthma, Hypertension, Cancer, COPD, Diabetes, and Heart
disease. The purpose of the reports is first to establish baseline
metrics for each disease category, then, over time, to measure
the changes in these metrics that may be the result of a plan
sponsor's disease management or wellness program.
|
Report Name
|
Definition
|
|
Age-Sex Analysis Report
|
Compares the group's age and sex cohorts with the benchmark
population and develops a composite Age.Sex factor for the group
to tailor benchmark data
|
|
DM Monitoring Report
|
Reports designed to provide healthcare cost and utilization
metrics focused on members with specific disease categories
typically included in a Disease Management program
|
|
Utilization Report
|
Shows the group's in- and out-of-network unit cost and utilization
data compared to custom benchmarks in as many as 40 user-defined
medical service categories
|
|
Trend Analysis Report
|
Shows the group's rolling 12-month and 3-month average PMPM
costs used to determine emerging PMPM cost trends
|
|
Rx Benchmark Scripts PMPM
|
Compares the population’s average scripts per member versus
the benchmark
|
|
Top 20 Rx Drugs
|
Compares the top 20 Rx Drugs prescribed with all other drugs
prescribed for the population
|
|
Rx Utilization Brand vs. Generic
|
Compares Total Prescriptions, Paid and Copay Amount by Drug
Type (Brand/Generic) for the selected population
|
|
Rx Therapeutic Class Avg. Cost
|
Summarizes the Paid Amount, Rx Scripts and Average Costs for
the Top 25 Therapeutic Classes
|
|
|